To give you a better understanding of how I use a combination of therapies to resolve chronic pain and recurring injuries I will share a case study of an Ironman competitor that came to me with a variety of problems that did not resolve after prior treatment and that prevented him from running, working out at the gym, and even limited him from participating in activities with his kids.

Stephen is a 45-year old father of two boys, Ironman competitor, and CEO of a successful Fortune 500 company. He had started running to get back in shape at the age of 39 and at that time also began working with a personal trainer. He was on the football team in high school and considered himself to be both very athletic and competitive. He mentioned to me that he was always very tight in his hamstrings and hip-flexors. He remembers not being able to touch his toes even in high school and after a knee injury from playing football – his movement was never quite the same.
Prior Treatment
Chiropractic Adjustments
Stephen came to see me after two years of bi-monthly chiropractic adjustments. While the adjustments initially helped with his low back pain – he would still feel stiff upon waking up in the morning and would experience pain after house repairs and playing a round of golf.
The chiropractor initially told him that he had type II degeneration in his lumbar spine and that the reduced disc space and misalignment of his spine (seen on x-rays) was what was contributing to his low back pain. He enjoyed running – but his chiropractor told him that he should limit his running until he purchased custom orthotics for his collapsed arches and pelvic imbalances.
While the custom orthotics eliminated the low back pain he was experiencing while running – he would still feel very stiff the next day and his back would still occasionally “go out” after a long run. The chiropractor remarked that he was the most inflexible person he had ever seen. In addition to the adjustments the chiropractor recommended that he should consider seeing a massage therapist and/or attend some yoga classes.
Massage and Yoga Classes
For the next six months Stephen visited a massage therapist once a month and attended weekly yoga classes. The massages definitely helped reduce his calf tightness and make him feel, “Like a hundred bucks” afterwards but the benefits quickly faded a week later. Yoga was also helpful – but he consistently struggled to get into the proper positions for many of the poses and would sometimes experience a low back flair up after the intense stretching.
Regular Personal Training
The personal trainer that Stephen worked out with once a week for the last couple of years seemed very skilled at putting together challenging workouts. The trainer had always advocated “getting stronger” as a remedy but workouts often seemed to be limited by Stephen’s poor flexibility. He stressed good technique during workouts but was unable to explain why Stephen would often feel worse after certain workouts.
While his personal trainer worked around his low back pain and hip tightness he eventually recommended that Stephen should see a physical therapist. His chiropractor agreed, despite telling him that he should continue to receive adjustments twice a month.
Physical Therapy
The physical therapist told Stephen that he had a weak core and that he needed to strengthen his abdominal muscles and low back. The recommended treatment was once a week for twelve weeks. Treatment involved soft-tissue work that included hamstring and hip-flexor stretching, low back stretches, and calf stretches.
After 15-minutes of soft-tissue therapy each visit he would receive electrical stimulation on his low back along with ice for ten minutes. The remainder of the session involved core stability exercises including planks, leg raises, situps, and bridges. He was given handouts of twelve different exercises that he was to perform at home every day.
Stephen began running again during this time but limited his distance to one or two miles at a time (no more than three days a week). He mentioned that he felt stronger but his low back had gotten even worse and he was now experiencing sciatica pain down his right leg. He was worried that maybe his running was the cause of this new pain.
His physical therapist told him that his chiropractor was probably right in that the degenerative changes to his spine were probably irreversible and that he would have to live with some degree of low back pain.
His physical therapist advised him to stop running for the time being and recommended that he continue treatment for twelve more visits. Frustrated he ended treatment after the twelve visits, worried that he would no longer be able to enjoy the activities that he once found so rewarding.
At this point, Stephen was about ready to give up running and accept what his chiropractor told him, “That he had a bad back and that the wear and tear at his age had taken its toll.”
Stephen found out about my practice after having a conversation with a runner that I had previously worked with. I helped her eliminate her plantar fasciitis and IT Band pain.
My Initial Assessment Findings
Stephen’s X-Rays revealed that he had reduced disc space between the vertebrae in his lumbar spine. His pelvis was anteriorly tilted which correlated to the exaggerated curve in his lumbar spine. However, these findings are the result of poor spinal stabilization – a common compensation pattern referred to as the Extension Compression Stabilizing Strategy (ECSS).
His X-Rays showed that there was great potential for improvement in his spinal alignment and movement. We would at some point discuss inherent limitations – but rather than showing what he couldn’t change – his x-rays demonstrated to me factors that he could change. This change in mindset was critical to our success in working together.
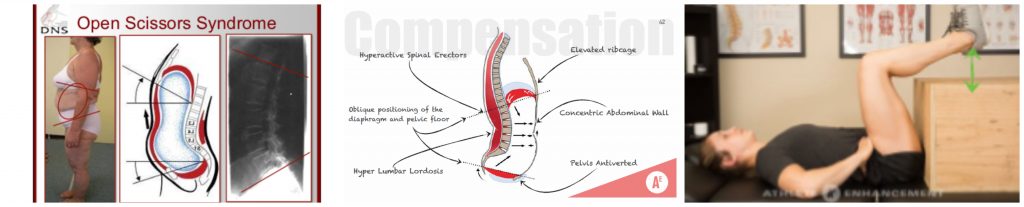
Extension Compression Stabilizing Strategy
Someone that relies on an ECSS has poor co-contraction of the hamstrings and deep abdominal muscles. They instead over-rely on the low back and hip flexors for stability. This perpetuates chronic tension in these muscle groups.
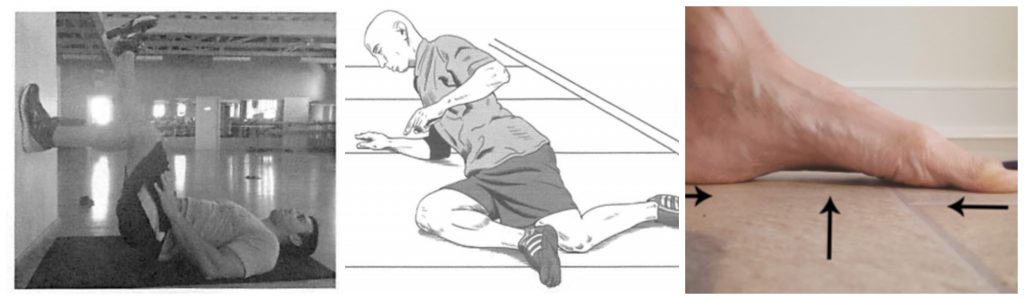
I put him in a 90-90 position (3rd image above) to gauge his ability to stabilize his spine – this immediately reproduced the low back pain that he often experienced.
Muscle testing revealed that he was in fact, relying on a compression strategy for stability. The muscles of his lumbar spine, in particular were overactive and compressing his low back – when he should have been utilizing his deep abdominals for stability.
The compression in his low back – was not merely related to arthritic changes but due to hyperactivity in certain muscle groups.
You have probably heard the expression, “Lift with Your Legs – Not Your Back.” The first image that comes to mind in this scenario is a rounded low back position (image 1) which represents one type of poor form during lifting. However, there is another compensation pattern that involves a hyperextended low back position while lifting (image 3).

It is this type of compensation that many athletes tend to favor – where the low back is over contracting creating an excessive lumbar curve. This movement dysfunction clearly reflected the spinal position seen on Stephen’s x-rays.
Dysfunctional Movement Patterns
Stephen was unable to disengage his low back during a full bodyweight squat which prevented him from pushing his hips back as his knees tracked forward. This requires hamstring engagement and a “letting go” of certain muscle groups like the hip flexors and low back.
I told Stephen that he should temporarily refrain from loaded squats because they involve maintaining a lumbar curve to ensure good form – but this type of movement, in his case would aggravate his low back. He told me that his trainer would have no problem substituting weighted single leg deadlifts for squats for the time being.
Stephen was also unable to touch his toes and had a severely limited straight leg raise – that I explained was not do to hamstring tightness but core instability and poor pelvic positioning. The ability to flex the hip in the toe touch and squat requires some degree of posterior pelvic tilt and posterior glide of the femur. The low back, lats, and hip flexors need to be able to temporarily relax (or inhibit) for this to occur.

I explained to Stephen that activities like leg raises, v-ups, overhead squats, and forward lunges (that over-recruit the hip flexors) should be avoided – until he could learn to inhibit his low back. Keeping an upright torso during squats and lunges would be counterproductive in his situation.
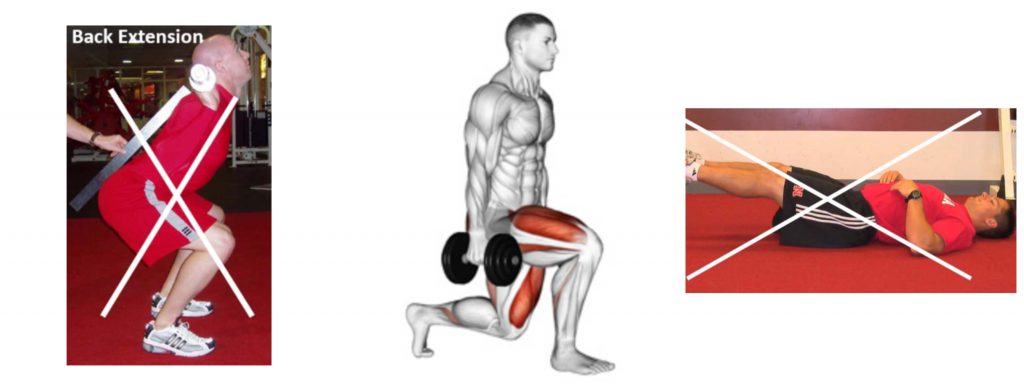
The “core stability and strength exercises” that his personal trainer and physical therapist prescribed were further reinforcing this dysfunctional ECSS pattern.
Even the bridges and plank exercises that he was prescribed were over-contracting his low back. Bridge exercises require that someone has adequate hip extension mobility and make it hard to activate the glutes and hamstrings with a relaxed low back.
Stephen’s low back was functioning as his hip – the hip extension needed during running was not coming from his hip but from his low back. His pelvis was stuck in an anterior tilt position that was limiting both hip flexion and hip extension movements.
Session 1: Finding and Feeling Hamstrings and Abdominals
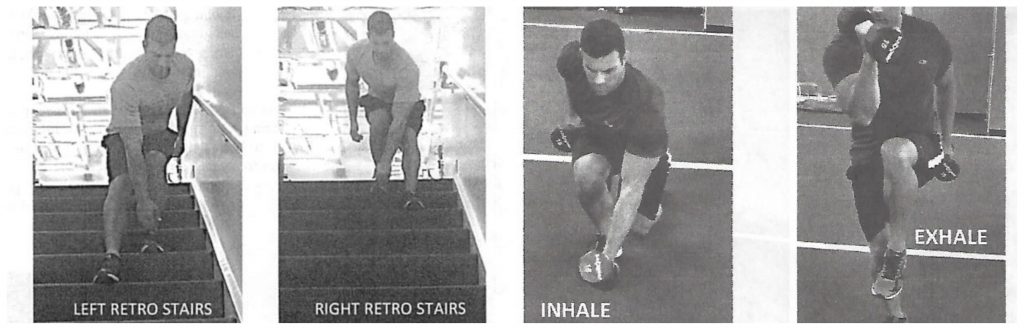
I gave Stephen a plank modification that would allow him to fully relax his low back and hip flexors and a hip lift to activate his hamstrings (with the hip more flexed than a bridge exercise). Reverse movements better engage the glutes and hamstrings so I gave him a reverse lunge exercise that would remove any stress from his low back. Lunging in reverse switches the activation pattern from the quads to the glutes and hamstrings.
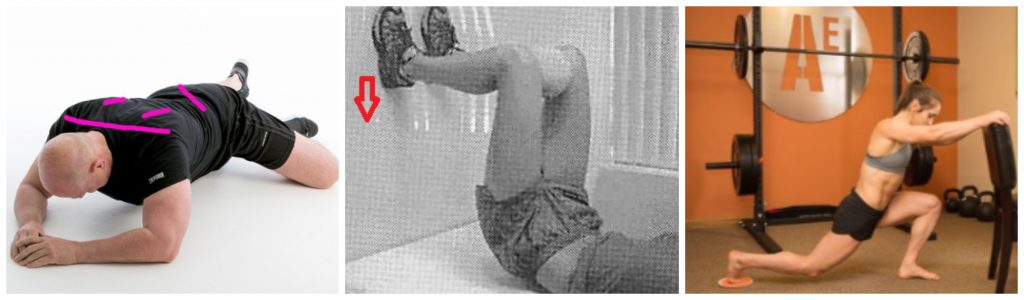
A big part of treatment at this point involved noticing the tension in his low back during various movements. I told him to exhale fully to engage his abdominals when getting into position for the exercises and to focus on finding his heels and feeling his abdominals and hamstrings engage.
I advised him to refrain from running until he completed two more visits. He was to incorporate the three exercises before his workouts with his personal trainer.
Session 2: Single Leg Stability
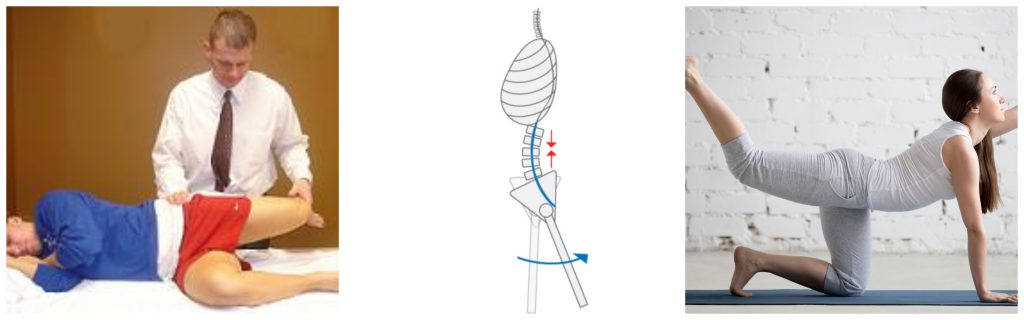
The first session focused on getting Stephen to find and feel his hamstrings in supported positions like the hip lift. He was learning how to engage his hamstrings and posteriorly tilt his pelvis (reverse lunge, hip lift) while learning to initiate movement from his hips/legs and not his low back.
At the beginning of the second visit (one week later) he reported to me that by relaxing his back he began to notice much better engagement through his hamstrings and abdominals.
The second visit focused on single leg exercises with the same principles in mind. I took him through a crossover exercise – a single leg progression of the hip lift.
Next, a side plank variation that would translate into better lateral abdominal activation for single leg stability in upright positions.
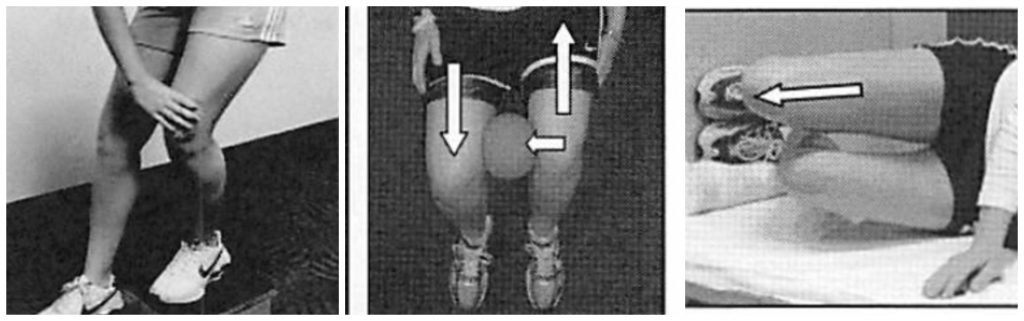
The third exercise was a “short foot” exercise that trains the muscles of the lower legs and feet to support the arch during single leg stance. He was to integrate the short foot exercise into single leg deadlifts with his trainer.
The remainder of the session involved Fascial Stretch Therapy to improve his range of motion and to get his body to feel end range positions that he would eventually need to control during his training.
At the end of the second visit he was able to fully extend his hips, perform a full toe touch (for the first time in years), and had no low back pain when I muscle tested his abdominal muscles and glutes.
Session 3: Improving Weight Transfer Between Legs
The first two sessions focused primarily on the sagittal plane – getting Stephen to relearn how to flex and extend his hips without over-recruiting his low back. His single leg stability greatly improved and the tension in his calf muscles, low back, hip flexors, and lats was gone.
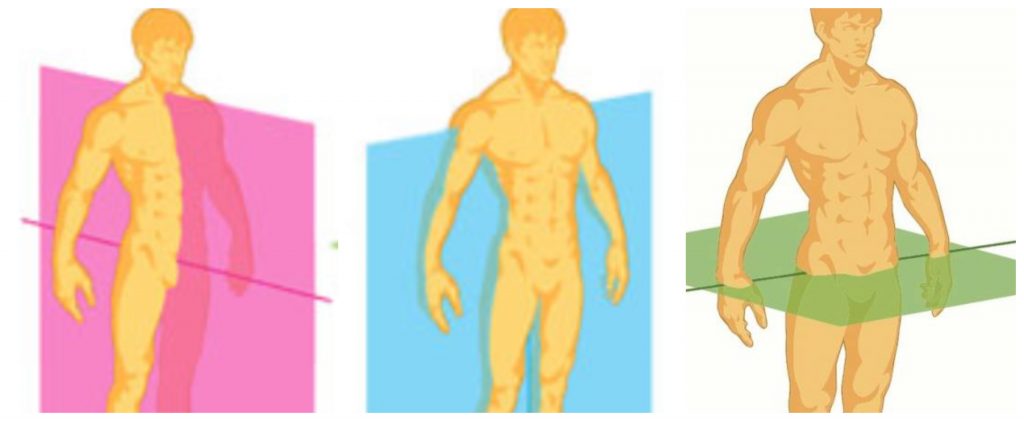
Running involves weight transfer between legs in the frontal plane. Stephen, like most runners, had a hard time shifting into his left hip and transferring his weight onto that side of his body.
His preference for standing on his right leg and loading his right leg while walking was contributing to both his compressed hip and low back on the right side of his body.
I performed some soft-tissue work to his left lower leg and ankle to help lift the arch of his left foot – which was still pronated. This correlated to the anterior pelvic tilt on the left side of his pelvis and his inability to properly load that left leg.
Stephen was surprised to hear that it is possible to restore the arches of severely pronated feet without the use of orthotics in many cases. This is possible through soft-tissue work, foot training, abdominal activation, and engagement of the muscles that stabilize the pelvis and leg.
His current exercises leading up to this session:
- Hip lift/single leg hip lift
- Modified front plank/side plank (low oblique sit)
- Short foot exercise integrated into reverse lunge
I then introduced three new exercises to help Stephen transfer his weight better over to his left side including a posterior capsule stretch for his left hip, a seated hip shift exercise (to do at work), and a scissor slide exercise.
Stephen was physically unable to fully shift into his left hip so I prescribed him a posterior capsule stretch after performing soft tissue work on his hips, adductors, and feet.
He was to maintain this new range of motion with the stretch and seated exercise at work. The scissor slide exercise would then integrate the muscle activation needed to stabilize his left leg after shifting into that hip. This exercise would reposition his pelvis to the left so that he could load that left while running (after the next visit).
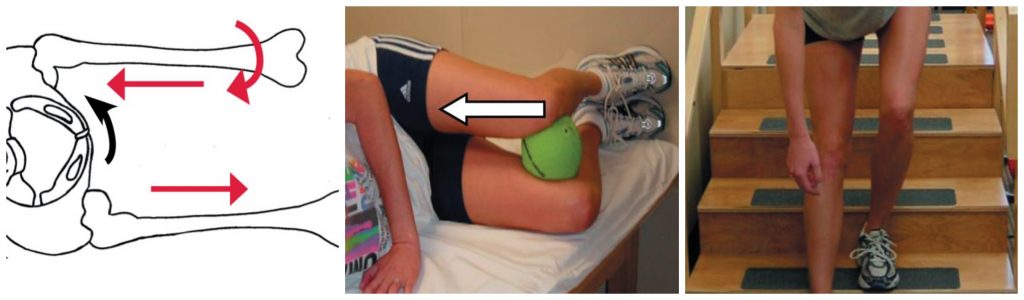
Despite Stephen’s rapid improvement I took him through a muscle test/orthopedic screen that gauges a runner’s ability to fully transfer their weight to one side. This test is scored from 0 – 5. Stephen scored a one on this test during his first visit and was now at a three.
I told him that once he was able to achieve a 4/5 on this test he would be ready to start going for short runs.

In the past Stephen was told to stop running without any valid performance metric that indicated his ability to stabilize his core and successfully transfer his weight between sides. This test demonstrated to him that he was on track to get back to running once he could pass this relevant metric for good running form.
The scissor slide exercise I gave him was intended to help him get from a three to a four on this movement screen. The next session would build upon this muscle activation pattern – integrating this activation into a more challenging upright position. Once he could maintain a score of a four – regardless of how he was ‘feeling’ that day he would demonstrate to me that he was ready to run.
Session 4: Integration of Upper Body Rotation
After performing the new exercises at home for a few days he reported to me that his sciatica and low back pain was now gone. He attended an outdoor activity that weekend that required a lot of walking and he woke up the next day with no pain or stiffness in his lower back.
The fourth visit focused on integrating better trunk rotation into upright activities like walking. I performed some deeper soft-tissue work during this session as well as assisted stretching to the muscles surrounding his ribcage to allow for better thoracic rotation to occur during his runs.
Now that he had better ground up support through his feet and was able to transfer his weight between sides – I worked with him on contralateral patterns that integrated arm swing with motion of the opposite leg.
At this point he was integrating the single leg hip lift, planks, reverse lunge, and scissor slide exercise into his warmup for his workouts. His trainer told him that he was, “like a new person” and was surprised at how his strength capacity had increased during his workouts just by integrating the four types of exercises into his warmup.
He easily scored a five on the assessment from the prior session and I told him that he was definitely ready to start running.
I gave him one new exercise to perform at home (retro walking) that involved walking up the stairs backwards and a backwards cross connect variation to include before his runs or personal training sessions.
Session 5: Building Endurance of Stabilizing Muscles
The first three visits were weekly, whereas session four and five were scheduling during his fourth week working with me.
He told me that he went for two three mile runs after the fourth session and for the first time in years did not have any discomfort during the run nor did he experience any pain or stiffness after.
I re-examined many of his movements during this fifth session and performed more advanced muscle testing that provided a greater challenge to his core stabilization. He did remarkably well on almost all of my assessments.
I then told him through a series of core stability endurance tests. He was able to hold the positions without pain but fatigued before reaching the desired thirty second mark. These performance indicators directly correlate to his ability to maintain good form during prolonged runs.

I advised him to limit his runs to three miles (as he had been doing) until he could hold each of the six positions for the desired thirty seconds.
Treatment Summary
Stephen continued to see me for more sessions after the initial five, but almost all of the expected changes he desired were accomplished within the four weeks.
The difference between his prior treatment and his work with me was my understanding of how movement dysfunctions perpetuate pain and injuries.
I outlined a plan of action with a realistic timeframe that allowed him to accomplish his goals. I re-assured him that he did have control over his situation and empowered him to take control of his situation by giving him exercises that were based on relevant assessment metrics and progressive treatment outcomes.
I made some modifications in the process and continually re-evaluated my treatment approach to ensure that I was on the right path with him to empower him to achieve his goals.
If you have sought out treatment in the past yet are still struggling with chronic pain or injury – there is hope. Oftentimes surgery is completely avoidable. To reassure you that what I offer is a realistic solution to your problem and re-establish TRUST in the process – I offer a FREE introductory running assessment.
Thank you for reading this case study – please contact me to schedule your session TODAY. I am committed to helping you redefine what’s possible – changes you can feel in minutes, not weeks.
The Runners Repairman